Interventional Bronchoscopy
( Page under construction )

Tracheobronchial foreign body aspiration (FBA) is a potentially life-threatening event because it can block respiration by obstructing the airway, thereby impairing oxygenation and ventilation. FBA in children may be suspected on the basis of a choking episode if such an episode is witnessed by an adult or remembered by the child.
What are the Signs and Symptoms ?
The signs and symptoms of FBA vary according to the location of the FB:
- Laryngotracheal – Laryngotracheal FBs are uncommon (5 to 17 percent of FBs) but are particularly likely to be life-threatening. Symptoms include stridor, wheeze, salivation, dyspnea, and sometimes voice changes. FBs in this location are most likely to present with acute respiratory distress, which must be addressed promptly.
- Large bronchi – The usual symptoms are coughing and wheezing. Hemoptysis, dyspnea, choking, shortness of breath, respiratory distress, decreased breath sounds, fever, and cyanosis may also occur. The right main bronchus is the most common location, followed by left bronchus and bilateral bronchi.
- Lower airways – Children with these FBs may have little acute distress after the initial choking episode
How to remove such Foreign Body ?
If Foreign body aspiration is known to have occurred or is strongly suspected, rigid bronchoscopy is the procedure of choice to identify and remove the object. Rigid bronchoscopy permits control of the airway, good visualisation, manipulation of the object with a wide variety of forceps, and ready management of mucosal haemorrhage.
Alternatively, flexible bronchoscopy is used to remove the FB in some centers with high levels of experience in this technique. This is done using biopsy, grasping forceps, balloon catheters, or wire baskets, with varying success rates. Potential advantages of using flexible bronchoscopy for FB extraction are avoidance of general anesthesia and the ability to reach subsegmental bronchi.

Endobronchial biopsy is used to obtain tissue under direct visual guidance from the tracheobronchial tree for histologic analysis. It cannot be used to biopsy lesions that cannot be seen using the bronchoscope.

Airway stenosis is a congenital or acquired narrowing that obstructs the passage of air to the lungs. Symptoms include stridor, wheezing, hoarseness, shortness of breath and respiratory distress. Patients who have severe airway stenosis are often dependent on a tracheotomy tube to breathe.
The most common cause of acquired airway stenosis is endotracheal intubation, resulting in 90% of cases. Other causes include external trauma, thermal or caustic injuries, chronic inflammatory diseases, infection, and rarely cancer.
This narrowed airway lead to difficulty in breathing and noisy breathing called as stridor. In such cases of subglottic stenosis or tracheal stenosis the narrowed area can be dilated using a balloon passed along side a bronchoscope.
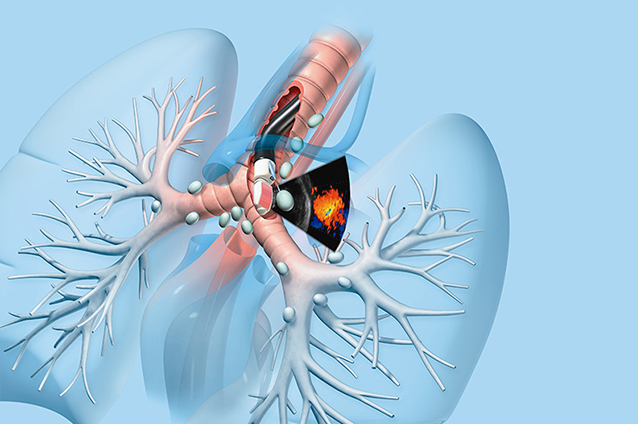
Endobronchial ultrasound (EBUS) is a bronchoscopic technique that uses ultrasound to visualize structures within and around the airway wall as well as the lung. The main advantage of EBUS guided sampling is that compared with surgical sampling, EBUS is a minimally invasive procedure that can be performed using local anesthesia and moderate sedation.
This process also involves taking a FNAC sample from lymph nodes of the chest. EBUS-TBNA is done through a special bronchoscope with has an ultrasound probe at its tip. This ultrasound can visualize the lymph node clearly. Once the lymph nodes are located a EBUS needle is passed through the channel of the bronchoscope and passed beyond its tip. The needle is then progressed into the lymph node and sample obtained under ultrasound guidance. The sample is then sent for detailed analysis including cytopathology and microbiology like cultures and genexpert MTB PCR.
